Guide to Fatty Liver Disease Treatment Approaches and Lifestyle Support
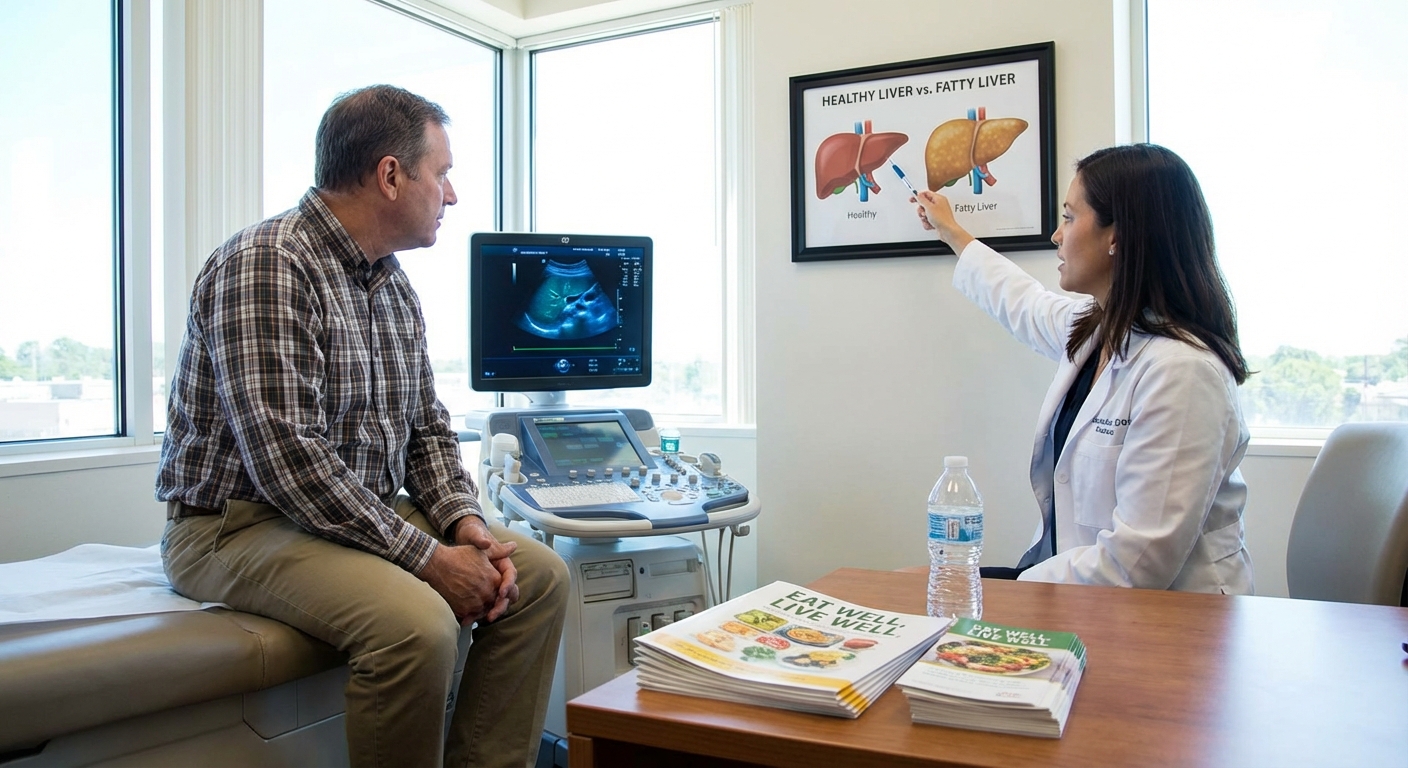
n “too much desk time.” When my doctor called and said, “Your liver enzymes are elevated; we should get an ultrasound,” my stomach dropped.
That ultrasound was my first real introduction to fatty liver disease.
Since then, I’ve gone down the research rabbit hole, tested lifestyle changes on myself, interviewed hepatologists, and pestered more than one dietitian. This guide pulls together what I’ve learned — the science, the lived experience, and the stuff people don’t always say out loud in a 10‑minute appointment.
What Fatty Liver Disease Actually Is (Without the Scary Jargon)
Fatty liver disease simply means there’s too much fat stored in your liver cells. Over time, that fat can trigger inflammation, scarring, and in some cases, progress to cirrhosis or even liver cancer.
There are two big categories:
- NAFLD / MASLD – Non‑alcoholic fatty liver disease (recently being renamed to MASLD – Metabolic dysfunction–associated steatotic liver disease). This is linked to weight, insulin resistance, type 2 diabetes, high cholesterol, and metabolic syndrome.
- Alcohol‑related fatty liver disease – Same idea (fat accumulation) but primarily driven by alcohol intake.
When I first read that up to 25–30% of adults worldwide have NAFLD (per studies summarized by the American Liver Foundation), I realized this isn’t some rare, obscure problem. It’s basically the liver’s version of a warning light on the dashboard.
The good news? In many cases, fatty liver is reversible, especially in early stages.
How Doctors Actually Diagnose It
In my case, the sequence went like this:
- Routine blood tests – Elevated ALT and AST (liver enzymes). Not specific to fatty liver, but a big nudge.
- Ultrasound – The tech quietly said, “Your liver looks a bit bright,” which is code for fatty infiltration.
- Rule‑outs – My doctor checked for viral hepatitis, autoimmune markers, medication side effects.
Common tools your provider may use:
- Blood tests – Liver enzymes, fasting glucose, HbA1c, lipids.
- Imaging – Ultrasound, sometimes CT or MRI.
- FibroScan (transient elastography) – A non‑invasive test that measures liver stiffness (scarring) and fat.
- Liver biopsy – Still the gold standard, but used when the diagnosis or severity is unclear, or when advanced disease is suspected.
One key nuance I learned from a hepatologist: you can have “normal” liver enzymes and still have significant fatty liver or even fibrosis. That’s why imaging and risk scores (like FIB‑4) matter.
Core Treatment Approaches: What Actually Moves the Needle
There’s no magic “fatty liver pill” right now for the average patient. The foundation is lifestyle and metabolic management. But that doesn’t mean “just lose weight and good luck.” Let’s break it down.
1. Weight Loss – But Targeted and Sustainable
When I tested different approaches, aggressive crash diets backfired: I’d lose quickly, rebound, and feel worse.
The research is pretty clear:
- Around 5% weight loss can reduce liver fat.
- 7–10% loss is often needed to improve inflammation and fibrosis in NAFLD/MASH (non‑alcoholic steatohepatitis) based on studies published in Hepatology.
What worked better for me (and what many liver specialists recommend):
- Aim for 0.5–1 pound (0.25–0.5 kg) per week.
- Think “long game”: 6–12 months, not 6 weeks.
- Combine food changes + movement rather than starving yourself.
The con: Progress is slower than influencer “shred” promises. The pro: This is the level of weight loss that actually shows up as less fat on liver imaging.
2. Nutrition: Less Sugar, Better Fats, More Fiber
I used to think fatty liver meant cutting all fat. Wrong. It’s more about the type of fat and the carb quality.
Patterns that are consistently liver‑friendly:
- Mediterranean‑style eating – Olive oil, nuts, fish, legumes, whole grains, tons of vegetables. Several randomized trials show it reduces liver fat even without major weight loss.
- Cutting added sugars and refined carbs – Sugary drinks, pastries, white bread, candy. Fructose‑heavy beverages (soda, some juices) are particularly rough on the liver.
- Prioritizing fiber and protein – Veggies, beans, lentils, oats, quinoa, plus lean proteins help keep you full and support weight loss without constant hunger.
Specific tweaks that made a difference for me:
- Swapping my nightly dessert for Greek yogurt with berries and nuts.
- Replacing sugary coffee drinks with black coffee or coffee with a splash of milk (fun fact: coffee itself is associated with lower risk of liver fibrosis in multiple studies).
- Keeping alcohol to near zero for several months.
Downside: You do have to read labels and say no to a lot of ultra‑processed “treats.” Upside: I noticed better energy within 2–3 weeks.
3. Exercise: It Doesn’t Have to Be a Marathon
I used to assume you needed intense workouts to touch liver fat. Turns out, moderate exercise alone can reduce liver fat, even without dramatic weight loss.
Evidence‑based sweet spot:
- 150–300 minutes per week of moderate activity (brisk walking, cycling, swimming).
- Add 2 sessions of resistance training (bodyweight, bands, or weights).
When I tested this, I started with a simple rule: 10,000 steps most days plus 2 strength days per week. My follow‑up ultrasound 9 months later showed significantly less fat, and my liver enzymes normalized.
Cons: Time and consistency. Pros: It’s free, boosts mood, and helps insulin sensitivity (which is tightly linked to fatty liver).
Medication Options: Where They Fit In (And Where They Don’t)
This is where nuance matters. For most people with early NAFLD, lifestyle changes are first‑line. But medications can help in specific scenarios.
1. Treating the Metabolic Drivers
Your doctor may prescribe meds to control:
- Type 2 diabetes – Metformin, GLP‑1 receptor agonists (like semaglutide / Ozempic, liraglutide), SGLT2 inhibitors.
- High cholesterol – Statins (atorvastatin, rosuvastatin). These are generally considered safe in fatty liver and can reduce cardiovascular risk, which is actually the leading cause of death in NAFLD patients.
Some GLP‑1 drugs have shown reduced liver fat and improved NASH in trials, likely because they drive weight loss and improve insulin resistance.
2. Liver‑Directed Therapies (Current and Emerging)
There’s a lot of buzz about new drugs for MASLD/MASH. As of my last deep dive:
- Vitamin E (800 IU/day) – For non‑diabetic NASH patients, some trials show histologic improvement, but there are concerns about long‑term high‑dose use (e.g., possible increased hemorrhagic stroke or prostate cancer risk). Definitely a “discuss with your hepatologist” situation.
- Pioglitazone – A diabetes medication that’s been shown to improve NASH in some patients, but comes with side effects like weight gain, edema, and possible bone fracture risk.
- Newer agents – Drugs like resmetirom (a thyroid hormone receptor‑beta agonist) and others are being actively studied; one has recently been approved in some regions for specific NASH cases. Access, cost, and long‑term data are still evolving.
Honest downside: Medications can help, but none replace lifestyle. And not everyone qualifies; many are reserved for biopsy‑proven advanced disease.
Alcohol, Supplements, and All the Grey Areas
When I asked my hepatologist, “Can I still drink?” she paused and said, “If your goal is to reverse this, I’d give your liver a break for now.”
Alcohol: How Much Is Too Much?
For NAFLD, even “moderate” alcohol can add fuel to the fire. Many experts recommend:
- Zero or near-zero alcohol if you have NASH, fibrosis, or cirrhosis.
- Very limited social drinking (and not daily) if your case is mild and your doctor agrees.
I went fully alcohol‑free for 6 months. Socially awkward at first, but my sleep improved and my labs got better. Worth it.
Supplements: Separating Hype from Help
Things I learned the hard way (and from PubMed at 2 a.m.):
- Milk thistle, turmeric, “liver detox” teas – Lots of marketing, very mixed evidence. Some supplements are contaminated or can actually damage the liver.
- Omega‑3s – Can help triglycerides and may modestly reduce liver fat, but they don’t fix inflammation or fibrosis on their own.
- Never assume “natural = safe” for your liver. Always clear supplements with your doctor, especially if you already have liver disease.
If a company promises to “detox your liver in 7 days,” that’s a red flag. Your liver doesn’t need a cleanse; it needs you to stop beating it up and support it consistently.
Lifestyle Support: Making Changes Stick in Real Life
The hardest part for me wasn’t knowing what to do. It was doing it consistently while juggling work, family, and stress.
Strategies that actually helped:
1. Tracking Without Obsessing
I used a simple app to:
- Log meals 4–5 days per week.
- Track steps and workouts.
- Snap periodic photos (weirdly motivating) instead of living by the scale.
2. Building a “Liver‑Friendly” Environment
- I stopped buying my “trigger” snacks for home.
- I prepped two default lunches for the week: grain bowl + protein, or big salad + beans.
- I put a cheap pair of dumbbells by the TV so I’d at least do something while watching shows.
3. Getting Social Support
When I finally told friends, “Hey, I’ve got fatty liver and I’m trying to reverse it,” something surprising happened: two of them said, “Me too.”
We shared recipes, step challenges, and lab updates. That made it feel less like a personal failure and more like a team project.
When to Take It Seriously (And See a Specialist)
Red flags that mean you shouldn’t just rely on Google and willpower:
- You already have type 2 diabetes, obesity, or metabolic syndrome.
- Ultrasound or FibroScan shows significant fibrosis.
- Liver enzymes stay high despite 6–12 months of effort.
- You’ve ever been told you might have cirrhosis.
In these cases, ask for a referral to a hepatologist (liver specialist). They can:
- Stage the disease more accurately.
- Discuss whether biopsy or advanced imaging is necessary.
- Talk through medications and clinical trial options.
I remember walking out of my liver clinic visit thinking, “This is serious, but not hopeless.” That’s the balance most people never get to hear.
The Bottom Line: Your Liver Is Remarkably Forgiving
What shocked me most was how responsive the liver can be when you change the inputs.
Within a year of:
- Losing about 8–9% of my body weight,
- Walking 8–10k steps most days,
- Strength training twice a week,
- Dramatically cutting sugar and alcohol,
my follow‑up testing showed my fatty liver had significantly regressed. I’m not a unicorn — this pattern is exactly what clinical studies report for many patients.
Is it easy? No. Does it require perfection? Also no.
If you’ve been told you have fatty liver disease, it’s not a moral verdict or a life sentence. It’s a loud, inconvenient message from one of the hardest‑working organs in your body: “I need backup.”
And with the right combination of medical guidance, realistic lifestyle changes, and a bit of stubbornness, that message can absolutely be answered.
Sources
- American Liver Foundation – Nonalcoholic Fatty Liver Disease - Overview of NAFLD, risk factors, and treatment approaches.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – NAFLD & NASH - Government resource with detailed medical information on fatty liver.
- Harvard Health Publishing – The rise of nonalcoholic fatty liver disease - Discussion of prevalence, risks, and lifestyle treatment.
- Mayo Clinic – Nonalcoholic fatty liver disease - Clinical perspective on symptoms, causes, and management.
- CNN Health – What to know about fatty liver disease - Accessible overview and expert commentary on fatty liver disease.



