Guide to Migraine, Depression, and Treatment Options
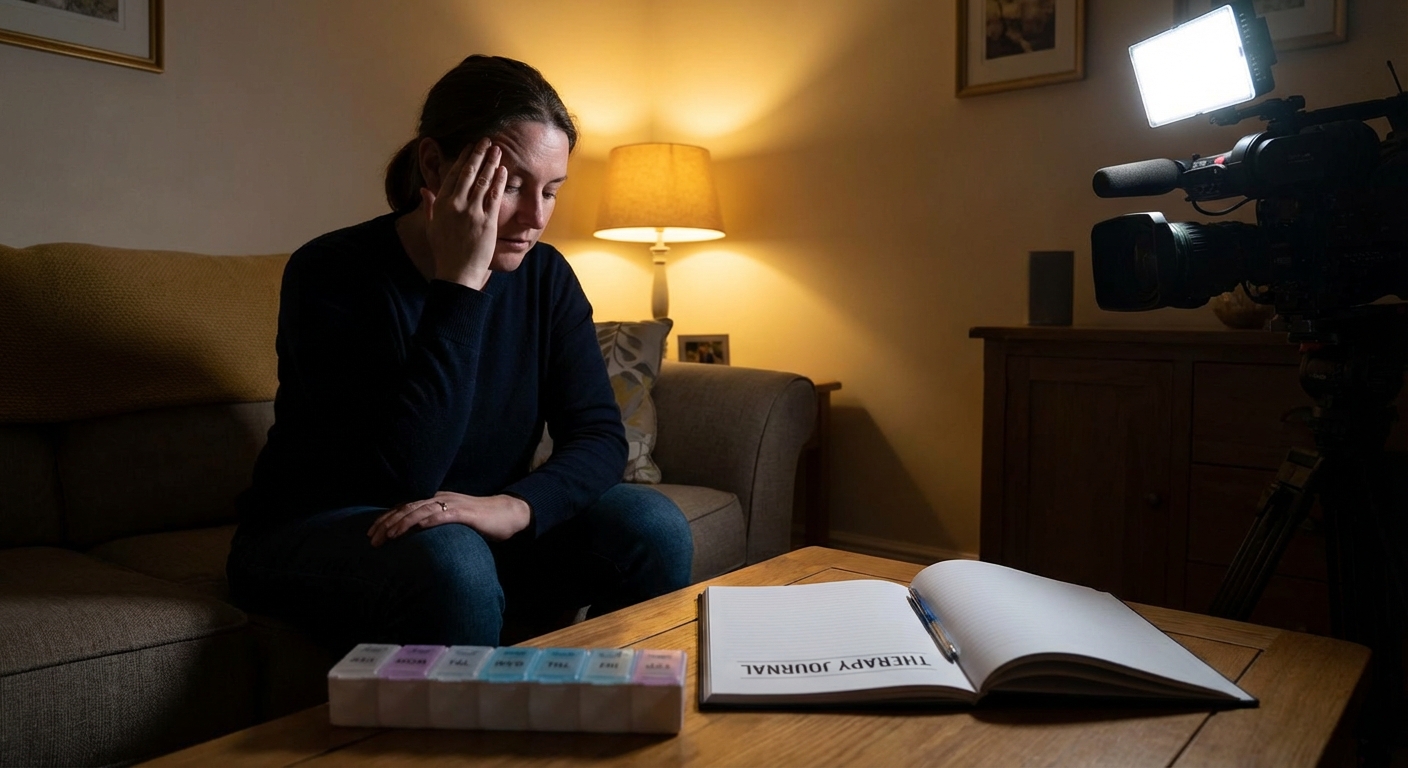
om floor, lights off, hands over my ears because the sound of my neighbor’s washing machine felt like a jet engine. I also hadn’t felt joy in weeks. That was the day a neurologist said two words that finally made everything click: migraine and comorbid depression.
I’ve been down the rabbit hole ever since—appointments, journals full of triggers, weird diets, meds that helped and meds that absolutely did not. This is the guide I wish someone had handed me at the start.
How Migraine Really Feels (Not Just “a Bad Headache”)
Migraine is a neurological disorder, not just a strong headache. When I was first diagnosed, my doctor put it bluntly: “Your brain is overreacting to normal signals.”
Typical migraine symptoms I’ve personally cycled through:
- Throbbing or pulsing pain, often on one side
- Nausea (I’ve often camped out near the sink, just in case)
- Sensitivity to light, sound, and even smells
- Brain fog so thick I’ve sent emails I barely remember writing
Some people (around 25–30%) get aura: visual zigzags, blind spots, or weird sensations before the pain hits. I’ve had auras where text on my laptop literally vanished from the middle of the screen.
The Science-y Bit (In Plain Language)
Researchers think migraine involves:
- Cortical spreading depression: a wave of electrical activity moving across the brain, followed by a suppression phase. It’s linked to aura.
- Trigeminal nerve activation: this nerve carries pain signals from the face and head; in migraine it gets loud.
- Neuropeptides like CGRP (calcitonin gene–related peptide), which amplify pain and inflammation.
The World Health Organization ranks migraine among the top causes of years lived with disability worldwide. That’s not exaggeration—that’s epidemiology.
The Quiet Tag-Team: Migraine and Depression
When I finally opened up to my neurologist about feeling emotionally flat and heavy all the time, she nodded like she’d heard it a thousand times. Because she had.
Studies show people with migraine are 2–3 times more likely to have depression or anxiety compared with those without migraine. It works both ways: depression can raise migraine risk, and frequent migraines can dig you into a depressive hole.
In my experience, the connection shows up in two ways:
- Emotional exhaustion from chronic pain
After my third migraine in a week, it wasn’t just my head that hurt. I’d start thinking things like, “What’s the point of making plans if I’ll just cancel again?” That chronic disability feeling slowly erodes your mood.
- Shared brain chemistry
Serotonin, dopamine, and norepinephrine play roles in both migraine and depression. That’s partly why some antidepressants can also help prevent migraines.
The scary part I wish more people talked about: people with migraine and depression together have a higher risk of suicidal thoughts. I’ve had days where it wasn’t that I wanted to die, I just desperately wanted everything to stop. That’s a huge red flag to get help, not something to tough out.
Getting an Actual Diagnosis (Not Just “Stress”)
When I finally saw a neurologist, here’s what the process looked like:
- Detailed history: When did headaches start? How often? How long? What helps? Any aura? Any family history? (Turned out my “sinus headaches” mom had were almost certainly migraines.)
- Migraine diary: I tracked sleep, hormones, weather, food, screens, stress. Patterns gradually appeared—like my “Sunday migraines” that were actually from changing my wake-up time on weekends.
- Rule-outs: Basic neuro exam and, in my case, an MRI—not because I had classic tumor signs, but because my migraines started somewhat abruptly in my 30s.
For depression, my primary care doctor used tools like the PHQ-9 questionnaire, plus a brutally honest conversation: how I was sleeping, eating, and whether anything felt enjoyable.
If you’re in this diagnostic limbo, two things really helped me:
- Writing down questions in advance. Brain fog makes you forget the important stuff.
- Bringing someone with me once. They noticed things I’d minimized.
Treatment Options for Migraine (What Helped Me and What… Didn’t)
Migraine treatment falls into two big buckets: acute (stop the attack) and preventive (reduce how often and how bad they are).
1. Acute Treatments: Surviving the Attack
I’ve tried pretty much the whole menu.
Over-the-counter medsIbuprofen, naproxen, and acetaminophen sometimes helped early on, but I quickly hit the “if I take this more than 10 days a month, I’m in medication-overuse territory” warning from my doctor. I ignored that once and ended up in a cycle of rebound headaches. Not worth it.
Triptans (like sumatriptan, rizatriptan)These changed my life at first. They target serotonin receptors and shut down migraine pathways. I still remember the first time: I took sumatriptan, lay down in a dark room, and 40 minutes later the pain dialed down like someone turning off a faucet.
Cons? They can cause chest tightness, tingling, and don’t play well with some heart conditions. I also can’t take them too often.
Newer meds: Gepants and ditansMore recently I tested ubrogepant, a CGRP receptor blocker. It was gentler for me—fewer side effects, more “oh, this is manageable now” than miracle cure. Friends I’ve met in migraine forums swear by rimegepant or lasmiditan instead. These are especially interesting for folks who can’t take triptans.
2. Preventive Treatments: Fewer Attacks Overall
This is where migraine and depression really start to overlap.
AntidepressantsI was prescribed amitriptyline first (a tricyclic antidepressant). Low dose at night. It did reduce my migraine frequency, but I woke up feeling like I’d slept in concrete. Dry mouth, weight gain, and a permanent “slightly hungover” vibe.
Later I switched to an SNRI (venlafaxine), which had solid evidence for both migraine prevention and depression. For me, that combo was more sustainable—fewer attacks and my mood climbed from “gray swamp” to “okay, I can do this.”
Beta-blockers (propranolol, metoprolol)These are blood pressure meds with good preventive data. When I tested propranolol, my heart rate calmed beautifully, but my energy tanked. Some people do great on it; I felt like I was living at 70% battery all day.
Anti-seizure meds (topiramate, valproate)Topiramate is famous in migraine circles for two things: effectiveness and side effects. It’s nicknamed “Dopamax” because of the brain fog. I lasted three weeks before the word-finding issues and fizzy-soda numbness in my fingers made it a no from me.
CGRP monoclonal antibodiesThese are the newer “migraine-specific” injectables like erenumab, fremanezumab, and galcanezumab. Once-a-month or quarterly shots that block CGRP or its receptor.
I finally tried one after arguing with my insurance for months. Result: My migraines went from 12–15 days a month to around 6–8. Not perfect, but a huge quality-of-life upgrade. Downsides: cost, occasional constipation, and the slight anxiety of injecting myself.
Treating Depression Alongside Migraine
Here’s where things get nuanced.
My psychiatrist and neurologist basically formed a tag team. A few key lessons from that experiment:
- One medication can sometimes hit both. Certain antidepressants (like SNRIs or some tricyclics) can improve mood and help prevent migraines. That’s efficient—but finding the right one is trial and error.
- Doses for depression vs migraine might differ. My venlafaxine dose for mood was higher than what some people use purely for prevention.
- Side effects matter even more with dual treatment. Anything that worsened sleep, anxiety, or fatigue tended to aggravate either my mood or my migraine threshold.
Therapy-wise, CBT (cognitive behavioral therapy) made an unexpected difference. Not because it erased pain, but because it gave me tools to manage the “mental spiral” when an attack hit: thoughts like “I’m useless” or “This will never get better.”
On weeks when I actually did my CBT homework, I noticed fewer full-blown depressive episodes, even if the migraine count didn’t change much. The brain is weirdly hackable sometimes.
Lifestyle Changes: The Not-So-Sexy Habits That Actually Help
I’ll be honest: when my doctor first suggested lifestyle changes, I rolled my eyes. I wanted a magic pill, not a lecture about sleep. But over a year of trial and error, this combo made a real dent:
Sleep (My Non-Negotiable)
I discovered that shifting my bedtime by more than an hour—especially on weekends—was like sending a personal invitation to a migraine. Now I:
- Wake up roughly the same time every day
- Aim for 7–9 hours, not 5 some nights and 10 others
It’s not glamorous, but it’s been one of the most reliable triggers I can control.
Food & Hydration
I tested the classic migraine trigger list: aged cheese, red wine, chocolate, processed meats, MSG. Turns out for me it’s not chocolate (thankfully), it’s skipping meals. A late lunch is almost always punished.
Keeping a food + migraine log for a month was annoying but clarifying. Some people do discover specific triggers like red wine or artificial sweeteners. Others don’t. Both are normal.
Movement and Exercise
Intense workouts triggered attacks for me, but gentle, consistent movement lowered my overall migraine and depression burden. A 30-minute walk most days felt doable and noticeably lifted my mood.
The trick: starting slow. Every time I tried to become a “new fitness person” overnight, I crashed.
Stress Management
“Reduce stress” is vague and slightly insulting when you’re drowning. What helped concretely:
- Short breathing exercises (4–7–8 breathing) before bed or during aura
- Saying no more often, even when guilt screamed at me
- A simple rule: on migraine days, I’m allowed to cancel guilt-free
No, breathing didn’t cure my migraine. But it shifted my nervous system from “perma-alert” to “slightly less on fire,” and that matters.
The Real Talk: What Doesn’t Work (or Is Overhyped)
In my experience—and this will ruffle some feathers:
- “Just drink more water”: Dehydration can be a trigger, sure. But chugging water during a full-blown attack has never once saved me.
- Random supplements without guidance: I tried magnesium, riboflavin (B2), and coenzyme Q10. Magnesium glycinate actually helped a bit with sleep and muscle tension. The others? Meh. And some “natural” migraine blends upset my stomach.
- Pushing through every attack: I used to pride myself on working through migraines. All that did was prolong recovery and worsen my mood.
None of this means those things never work. It means they’re not universal cures and they can waste precious time and hope if you expect miracles.
When to Seek Urgent Help
A few red flags my doctors drilled into me:
- A sudden, severe headache that feels like “the worst of your life”
- Headache with fever, stiff neck, confusion, or seizures
- A big change in your usual migraine pattern
- Any thought of self-harm or feeling like you “don’t want to exist anymore”
I’ve gone to the ER once for a “this feels different and terrifying” headache. It turned out to be a nasty but benign variation, but I don’t regret going for a second.
If your thoughts are turning dark, that’s not weakness—it’s a symptom, like nausea or light sensitivity. It deserves serious, immediate care.
Living With Both: A Hopeful, Messy Middle
My life didn’t magically transform once I had a diagnosis. I still cancel plans. I still have days where my brain feels like scrambled eggs. But I also:
- Have fewer migraines than I used to
- Spend less time in bed in a dark room
- Bounce back from depressive dips faster
The biggest shift for me was stopping the “all or nothing” thinking. Instead of aiming for zero migraines and perfect mood, I now aim for:
- Fewer attacks
- Shorter duration
- Less emotional fallout
That’s achievable. And it’s made my life recognizably mine again.
If you’re dealing with migraine, depression, or both, you’re not imagining it, you’re not weak, and you’re absolutely not alone. With the right combo of meds, habits, and support, your brain can become a much less hostile place to live.
Sources
- NIH – Migraine Fact Sheet - Overview of migraine as a neurological disorder, symptoms, and treatments from the U.S. National Institute of Neurological Disorders and Stroke.
- Mayo Clinic – Migraine - Detailed clinical explanation of migraine, risk factors, and medical management.
- National Institute of Mental Health – Depression - Evidence-based information on symptoms, diagnosis, and treatment options for depression.
- American Migraine Foundation – Migraine and Mental Health - Discussion of the connection between migraine and mood disorders, including depression and anxiety.
- Harvard Health – New Treatments for Migraine - Overview of CGRP-targeted therapies and other emerging migraine treatments.



