Guide to PrEP Cost Assistance Resources and Program Eligibility
rching every assistance program I could find. When I finally sat with a case manager and walked through the options, I honestly couldn’t believe how much money people are leaving on the table just because the system is confusing.
So if you’ve ever thought, “PrEP sounds great, but there’s no way I can afford it,” this guide is for you.
I’ve helped a few friends navigate PrEP coverage over the last couple of years, and every single time, the pattern is the same: fear about cost, confusion about programs, and then massive relief when we realize they’ll probably pay close to nothing—or literally nothing—out of pocket.
Let’s walk through what I’ve learned, step by step.
Quick refresher: What is PrEP and why is it so pricey?
PrEP (pre-exposure prophylaxis) is a medication strategy that helps prevent HIV. The two main oral options approved in the U.S. are:
- TDF/FTC (brand name Truvada, plus generics)
- TAF/FTC (brand name Descovy)
There’s also injectable PrEP (cabotegravir, brand name Apretude), which is given every 2 months.
When I first looked up the “list price” for brand-name PrEP, my jaw dropped: we’re talking $1,600+ per month retail for some brands in the U.S. Generic Truvada is cheaper, but still often a few hundred dollars monthly if you’re paying cash.
The twist? Almost nobody who knows how to use assistance programs actually pays that much.
The 3 big buckets of PrEP costs
When I tested different scenarios with friends—uninsured, high-deductible plans, Medicaid—the cost questions always fell into three buckets:
- The drug itself (the PrEP medication)
- Lab work (HIV tests, kidney function, sometimes STI and hepatitis tests)
- Clinic visits (telehealth or in-person)
Different programs cover different pieces. The magic is stacking them the right way.
1. Using insurance: how far does it actually go?
Private insurance / employer plans
After the U.S. Preventive Services Task Force (USPSTF) gave PrEP an “A” rating in 2019, most private insurers were required under the ACA to cover it without cost-sharing for people who qualify.
What that usually should mean:
- $0 copay for the PrEP medication (often generic TDF/FTC)
- $0 cost for associated labs and visits that are part of PrEP preventive care
In my experience, this doesn’t always play out perfectly. I’ve seen:
- Plans cover the drug but bill labs as “diagnostic” instead of “preventive”
- Prior authorizations that drag on
- Pharmacies that default to brand-name when generic would be free
What helped the most:
- Asking the prescriber to write “generic TDF/FTC for PrEP” explicitly
- Calling the insurer and asking which PrEP NDCs are covered at $0 preventive
- Using a PrEP clinic or LGBTQ+ health center that knows how to code visits correctly
Medicaid and Medicare
When a friend on Medicaid applied for PrEP, I was shocked how smoothly it went comparatively.
- Medicaid: Many state Medicaid programs cover PrEP with minimal or no copays. Some states layer PrEP Drug Assistance Programs (PrEP-DAPs) on top.
- Medicare: It’s trickier. Medicare Part D may cover PrEP, but you might still face deductibles or coinsurance unless you qualify for Extra Help (Low-Income Subsidy) or a manufacturer program.
Always check your state’s health department or Medicaid site—they often spell out PrEP coverage pretty clearly.
2. Uninsured or underinsured? Here’s where assistance programs kick in
This is where most people think they’re out of luck… and they’re usually wrong.
Manufacturer Patient Assistance Programs (PAPs)
If you’re uninsured or your insurance refuses to cover a specific brand, Patient Assistance Programs can sometimes get you PrEP medication for free for 12 months at a time.
Examples:
- Gilead Advancing Access (for Truvada and Descovy)
- ViiVConnect (for Apretude in some cases; also supports HCPs navigating coverage)
How these usually work in practice:
- You must be uninsured or underinsured, and meet income requirements (often up to 500–600% of the federal poverty level)
- You or your provider fill out a form (online/fax) with proof of income
- Once approved, the drug is shipped to your pharmacy or clinic
I went through this with a friend who’d just aged off their parents’ insurance. They were sure they’d have to stop PrEP for months. Their approval through a manufacturer PAP took about 5 business days, and their out-of-pocket drug cost dropped to $0.
Copay assistance for insured patients
If you have commercial insurance but high copays, copay cards can wipe most of that out.
Typical setup:
- You sign up online
- You bring a card (virtual or printed) to your pharmacy
- The copay card pays part or all of your copay, sometimes up to a yearly maximum (e.g., $7,200/year, depending on the program)
Catches I’ve run into:
- Not usable with Medicaid or Medicare due to federal anti-kickback rules
- Some plans use “copay accumulator” policies, where the copay card doesn’t count toward your deductible
Still, for many privately insured folks, these cards turn a $200+ monthly copay into $0–$10.
3. State PrEP Drug Assistance Programs (PrEP-DAP)
This is the little-known gem.
Some states run PrEP Drug Assistance Programs that function a bit like HIV ADAP, but for people who are HIV-negative and at risk. These programs may cover:
- The PrEP medication itself (if not covered elsewhere)
- Lab costs
- Clinic visit copays
Eligibility typically includes:
- Residence in that state
- HIV-negative status
- Income below a set threshold (often 300–500% FPL)
When I dug through state health department websites, a few stood out for clear PrEP-DAP info:
- New York, Massachusetts, California, Washington, and Illinois all have strong PrEP support structures.
If you’re not sure your state has one, search: `"[Your State] PrEP DAP"` or check your state’s HIV/STD program page.
I’ve watched case managers layer this on top of manufacturer PAPs and insurance to get people truly zero-dollar coverage—meds, labs, and visits.
4. Community clinics, telePrEP, and 340B programs
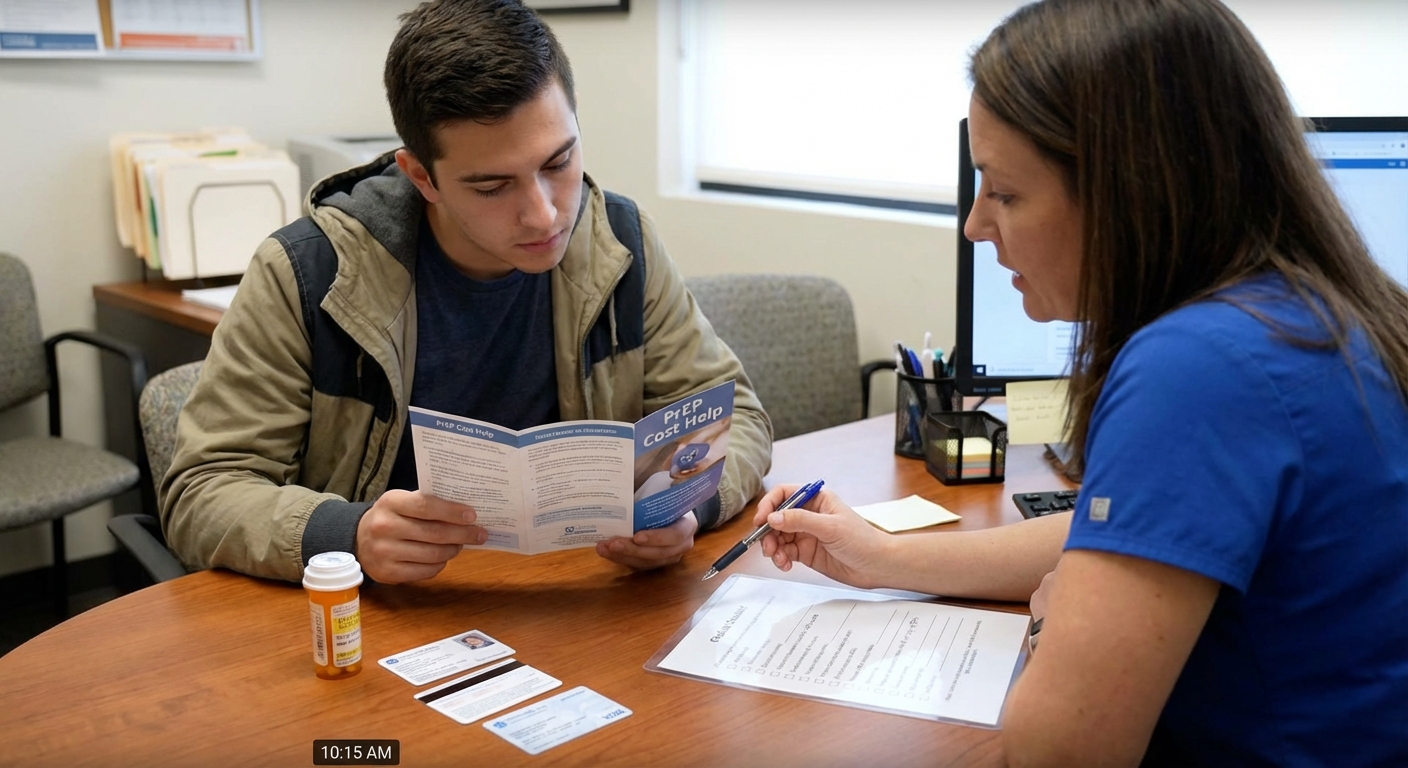
One detail I didn’t fully appreciate until I visited a community health center: some clinics are basically experts in hacking the system on your behalf.
Many LGBTQ+ clinics, sexual health centers, and FQHCs:
- Use 340B drug pricing to discount meds internally
- Have staff whose full-time job is helping you apply for PAPs, PrEP-DAPs, and insurance
- Run telePrEP programs with mailed labs and meds, often at ultra-low cost
In my experience, when someone is overwhelmed, sending them directly to a local LGBTQ+ clinic or PrEP-specific telehealth service is the most effective move.
5. Who’s actually eligible for PrEP assistance?
Here’s the part that surprises people: you don’t have to fit a stereotype to qualify. Eligibility is based on risk and finances, not identity.
Clinical eligibility (for PrEP itself)
The CDC and USPSTF guidelines generally recommend PrEP for people who:
- Have anal or vaginal sex with partners of unknown HIV status, especially without condoms
- Have a partner living with HIV who’s not consistently virally suppressed
- Have had a recent bacterial STI (like syphilis, gonorrhea, or chlamydia)
- Inject drugs and share equipment
You’ll need:
- A negative HIV test before starting
- Periodic follow-up tests every 2–3 months (depending on regimen)
Financial eligibility (for assistance programs)
This is where each program differs, but common patterns include:
- Income caps – often 300–600% of the federal poverty level
- Insurance status – PAPs usually for uninsured; copay cards for privately insured
- Residency – for state programs, you must live in that state
One friend assumed they “made too much” to qualify. Turned out they were just under 500% FPL for their household size and got approved.
Moral of the story: always check the actual numbers instead of guessing.
6. Pros, cons, and real-world frustrations
I wish I could say this system is smooth and logical. It’s… not. Here’s my honest breakdown from watching people go through it.
What works well:- When you connect with a clinic that knows PrEP inside out, the process feels almost turnkey.
- Many people can get PrEP meds at no cost if they’re willing to fill out forms.
- Generic PrEP has made insurance coverage much easier.
- Paperwork overload—faxing forms in 2026 still feels wild.
- Inconsistent pharmacy knowledge: I’ve seen pharmacists tell people, incorrectly, that a copay card can’t be used.
- Gaps in coverage for labs and provider visits, especially for the uninsured.
- Injectable PrEP (Apretude) has more coverage headaches and prior auth battles.
Even with those flaws, when I compare “no PrEP because cost seems scary” versus “two afternoons of paperwork and then nearly-free PrEP,” the math speaks for itself.
7. A practical roadmap if you’re starting from scratch
If I were helping you one-on-one, here’s the basic sequence I’d walk you through.
- Figure out your insurance status
- Insured privately? Check if your plan covers generic PrEP at $0 as preventive.
- On Medicaid? Call or check your state site for PrEP coverage.
- Uninsured? Plan to lean on PAPs + community clinics.
- Find a PrEP-savvy provider
- Search for local LGBTQ+ clinics or sexual health centers.
- Or use a dedicated telePrEP service operating in your state.
- Ask specifically about financial navigation
Say something like: “I’m interested in PrEP, but cost is a barrier. Do you have staff who help with assistance programs?”
You’d be surprised how many places answer: “Yes, absolutely.”
- Apply for the right program(s)
- If uninsured: manufacturer PAP + (if available) state PrEP-DAP
- If insured with high copays: copay card + possible state help
- Double-check labs and visit coverage
Don’t just ask, “Is the medication covered?” Also ask, “How are my labs and follow-up visits billed?”
8. When the system fails: realistic backup options
Sometimes, even with all this, people hit walls—especially in states with limited safety nets.
In those cases, I’ve seen a mix of alternatives:
- Sliding-scale visits at community clinics
- Cash-pay labs using discount services (often much cheaper than hospital pricing)
- Short-term PrEP “bridging” programs run by health departments or nonprofits
These aren’t perfect, and they don’t replace a solid long-term plan, but they can keep someone from falling completely off PrEP during gaps in coverage.
Final thought: Don’t self-disqualify
The biggest barrier I keep seeing isn’t technically money—it’s assumption. People assume they won’t qualify, or it’ll be too complicated, or they “don’t deserve” help because they’re not poor enough or risky enough.
When I actually sit with folks, pull up the forms, and run through the numbers, they’re almost always eligible for something meaningful.
If you take nothing else from this guide: don’t rule yourself out before you’ve checked your options. Get a PrEP-friendly clinic or navigator in your corner, and let them do what they’re good at—finding ways to make prevention affordable.
Sources
- CDC – Preexposure Prophylaxis for the Prevention of HIV Infection in the United States: 2021 Guideline – Official U.S. clinical guideline for PrEP use and monitoring
- U.S. Preventive Services Task Force – Recommendation: Prevention of Human Immunodeficiency Virus (HIV) Infection: Preexposure Prophylaxis – Details on the “A” rating that drives no-cost coverage
- HIV.gov – Pre-Exposure Prophylaxis (PrEP) – Federal overview of PrEP, access, and assistance options
- Gilead – Advancing Access Program – Official site for Truvada/Descovy patient assistance and copay support
- Kaiser Family Foundation (KFF) – Coverage of HIV Prevention Drugs – Analysis of how commercial plans cover PrEP and related services



